This November, my wife and I checked off a depressing anniversary: one year of trying for a baby. As two halves of a same-sex marriage, both of us women, we’ve been in doctor’s offices for the past year undergoing IUI, or intrauterine insemination. A year might not sound like a long time in that sense, but in terms of money and effort and knowing we’ve had perfectly timed attempts again and again, it feels like an eternity. When we first started this process, technically there was no “infertility” diagnosis; we were just a same-sex couple who always knew we’d at least need assistance in acquiring sperm, if nothing else, or so we thought. But it’s become more complicated than that.
The procedure of IUI is performed in a doctor’s office. The short story of what happens is that when your body is ready for ovulation, which can mean medications for days before that to stimulate the ovaries, an injection is performed that prompts ovulation and you release one or more eggs depending on how many have grown to maturity (typically one, but sometimes more on medication). About a day after that injection is given, a doctor uses a speculum to open the cervix and a catheter (flexible, tubey thing) to insert the sperm directly into the uterus, not just into the vagina. So fun! The goal is for those sperm to swim up into the Fallopian tube, meet the egg, and then for the fertilized egg to descend, implant in the uterus and grow. We are using donor sperm purchased through a sperm bank, which is pricey and can be hard to acquire (our donor has a waitlist that took us months to get on), so we decided to basically get straight into a fertility center to make sure we had professional, medical support as we tried to conceive.
It’s hard to talk about this process for a variety of reasons; mostly, because it hasn’t worked yet, but also because trying to have a baby is incredibly personal no matter how you go about it. It’s intimate and important whether you’re at home or in a doctor’s office. Also, most stories of infertility are told at the end, after success has been achieved. I want to share from the middle, the dead center of the mess, still trying to navigate through the storm. We’re not at the finish line yet and I don’t know how long it’ll take or what method will finally get us to the other side, where we get to become parents. I’ve stopped trying to guess. But this isn’t a situation that is valid only once you’ve achieved the goal. We’re in the hard part, and that’s an important perspective to be standing in. We are in crying-on-the-couch, going-through-it mode. We always knew we would need some help getting pregnant since we’re both women and lack “access to sperm,” as our doctor hilariously put it, but we were not prepared for the length of time it’s taken, the ups and downs of the process along the way, and how much of the unknown we would face that I had absolutely no concept of before we started.
The Doctors Know A Lot, But Not Everything
Even with two uteruses, great doctors, and good odds, every case is different and the treatments aren’t foolproof. There is a lot of guesswork involved about how your body will respond to certain treatments and hormones and it doesn’t always happen the way you, or your doctor, expect. Even with drugs, and ultrasounds, and doctors we trust, we’ve had round after round of failed intrauterine inseminations. And the worst part is that, most of the time, the exact reason why is unknown. It could be the egg, or an insufficient uterine lining, or something else entirely. The egg could have been fertilized but failed to implant, or the egg and sperm could have failed to fertilize at all. Even when you know the exact day of ovulation, the size of the follicle down to the millimeter, or the precise thickness of the uterine lining, the reason it still doesn’t work isn’t always clear. It can take time and a lot of effort to create the perfectly balanced cocktail of medications, timing, and internal environment to make things work, and there are more factors than I ever realized.
The Roller Coaster Your Month Will Become
It’s not just the infamous TWW that’s difficult, which is the two-week waiting period after insemination is performed when you’re waiting to get, or miss, your period. There are doctor’s visits to check your follicles to make sure they’re maturing at the right rate, evaluate uterine lining levels, and did I mention every single one of those visits involves a vaginal ultrasound? None of this is happening in those cute abdominal ultrasounds like in the movies where they squeal and giggle because the gel is too cold. It’s way too early on for abdominal ultrasounds, which means every single appointment, there’s a probe inserted vaginally. The doctors are good at it, but even so, it’s like having a Pap smear three times a week. Most people don’t even mention that part in the struggle to get pregnant, which is a testament to the fucking strength of people with uteruses. It’s such a hard process already that being subjected to invasive vaginal examinations day in and day out just becomes part of the gig. But I’ll tell you about it, because I’m not tough, and I love to complain. And it’s not just uncomfortable and inconvenient: it’s an upheaval of your whole day-to-day life. I kind of just thought we’d live normally, come in on the day of insemination, and then get pregnant and move on. And for some people I’m sure that’s true, but not for us. There are consults and tests, and meds that work and meds that don’t, and then appointments and procedures, and more tests. Each little piece of news, good or bad, can derail your day, or week, or month.
Expect The Unexpected
If someone had told me that after a year of attempts, we’d be moving on to other even more expensive, invasive methods because no one was pregnant yet, I would have cackled. Two healthy women, both under the age of 30 when we started, using high-quality donor sperm. It seemed like we’d get pregnant in the first few rounds. Then, we didn’t, and half a year had somehow passed by. We had another unwelcome surprise when blood tests and ultrasounds diagnosed me with PCOS, which stands for polycystic ovary syndrome, and can manifest in different ways but for me tends to result in my body ovulating on a very irregular schedule, or not at all, which means I need more help getting pregnant and probably would even if I were in a straight relationship. We always knew we’d need sperm, but to need this much medical help in trying to conceive is unexpected. And those are big picture surprises. Smaller picture, there have also been roadblocks. One medication resulted in me developing between four and six mature follicles, which is so many my cycle was nearly canceled. Another medication resulted in me having an ideal uterine lining measurement for pregnancy, but no follicles ready to release a mature egg, so back to square one we went, reversing all the gains made in my uterus in the process. Every person with a uterus is different, and while I may be especially tricky, I have been consistently and genuinely surprised by how difficult it’s been to wrangle my cycle and my body. Coming into this with an admittedly casual mindset, adjusting to the big picture reality as well as riding the smaller waves, has been intense.
The Most Difficult Part Isn’t The Money, Although That Part Does Suck
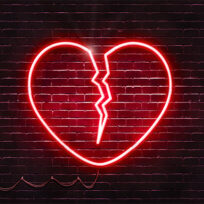
You know the quote, the definition of insanity is doing the same thing over and over and expecting different results? That sums up going through infertility treatments. It’s the biggest leap of faith out there. You are trying to make something out of basically nothing, or at the very least, out of microscopic body parts you can’t even see, and then hoping it sticks. You are trying to create actual life over and over again. And when it doesn’t work, that loss is felt like just that: a loss. You technically can’t lose something you never had, but that carved-out feeling of pain is still there as the future you’re trying so hard to move toward just takes another step away from you. The more times you try, the harder it is, because you start having to deal with problems you could easily avoid if you were already pregnant. Just shipping donor sperm to our clinic alone costs hundreds of dollars. Ordering new medications for another attempt. Trying to calculate how much sperm is left, how many more vials we’ll need, trying not to panic at how many we’ve gone through already just in the process of trying, with nothing to show for it until someone is pregnant. There’s no moving on to the next step of our lives until we can surmount this one. If we were already pregnant, we could start thinking about buying baby stuff and telling our families and moving on to the fun parts. Instead, every negative test is like a step backward. It means another try, another month—at least—of money and time and procedures. Yet, we do it. We try again and again. And I’m proud every time. It’s brave to try again where you’ve just failed. If I’d known how long this would take and how complicated it’s been, I might have been afraid to try at all. A lot of the adjustment has just been accepting that I don’t know when it’s going to happen or when it’s going to work. There is some comfort in knowing we’re doing the best we can.
My wife said the other day that you cling on to the good stories, the ones you hear about where couples get pregnant the first try or early on, and you push the bad ones away and just hope your story will be one of the easy ones. I’ve lost faith many times this year and there have been times it felt like I was free-falling into an abyss. What I’ve tried to remember is that we are not on the edge of a cliff. We’re on a bridge. We’re taking steps to get to the other side. That’s sometimes all you can do.
Image: Sergey Filimonov /Stocksy.com